- Anesthesiology Malpractice
- Posts
- Malignant Hyperthermia - Was Treatment Delayed?
Malignant Hyperthermia - Was Treatment Delayed?
Case #21
A 54-year-old man presented to the hospital for a right total knee replacement.
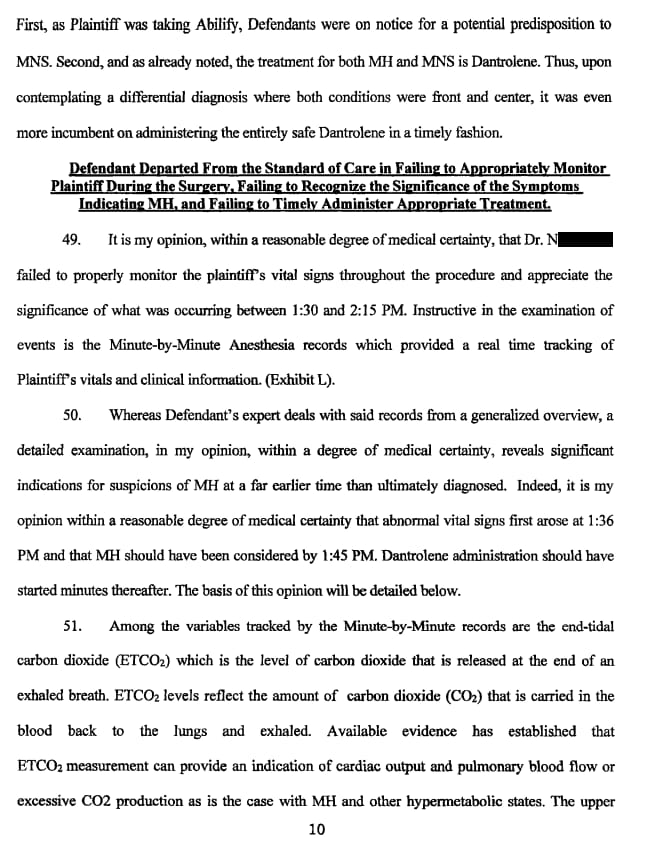
His medical history was significant for bipolar disorder on Abilify.
He had no prior anesthetics, and no history of family problems with anesthesia.
After a discussion of risks and benefits a spinal was performed, but the patient was not getting numb.
After 10 minutes he was converted to GA.
The sevoflurane vaporizer was turned on at 11:35AM.
Temperature was monitored with an esophageal probe, heart rate and ETCO2 remained normal throughout the case.
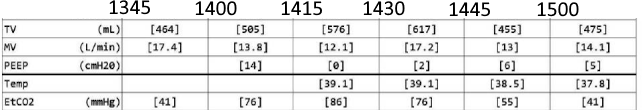
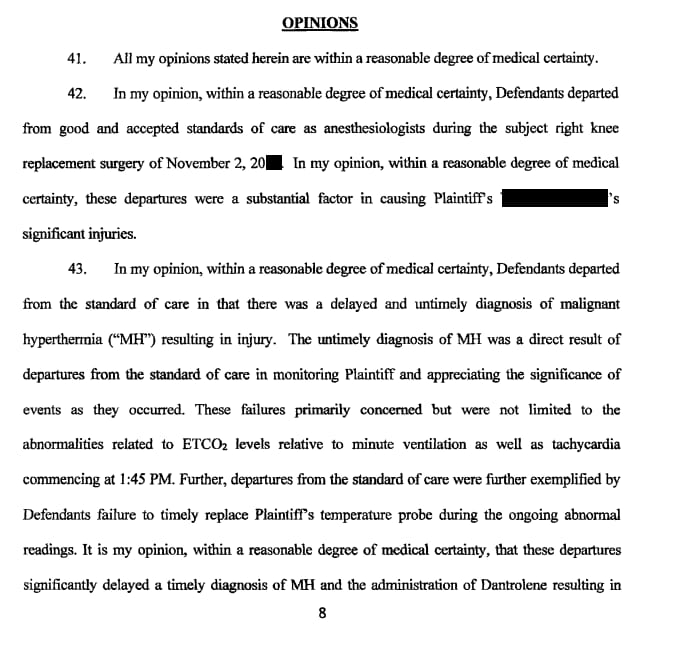
At 1:34PM the tourniquet was released and ETCO2 rose to 66mmHg before falling to 27mmHg over the course of 15 minutes. It then began to steadily rise.
The patient also became tachycardic at this time sustaining a HR > 100bpm.
The patient was not arousable throughout emergence and instead remained tachycardic with an increasing ETCO2.
At 2:00PM the anesthesiologist called for assistance and 2 anesthesiologists responded.
The esophageal probe was replaced as it had been removed for emergence.
There was a brief discussion of MH versus neuroleptic malignant syndrome (NMS).
The MH cart was brought in the room and dantrolene first given at 2:19PM. The patient would receive 4 boluses of 250mg in the OR.
Other measures included bicarb administration, cooling with ice and cold fluids, A-line and CVC insertion.
Temperature and ETCO2 stabilized around 3:15PM.
The patient was transported to the ICU where he received additional dantrolene.
He was extubated 12d later.
He went on to require occupational therapy and swallow therapy.
He went to subacute rehab for 2 weeks.
Upon discharge from rehab he was back to his baseline and had no residual neurocognitive or physical defects from his MH episode.
Improve your practice by reviewing malpractice cases.
Join thousands of anesthesiologists on the email list.
He sued, naming 2 of the anesthesiologists and the hospital.
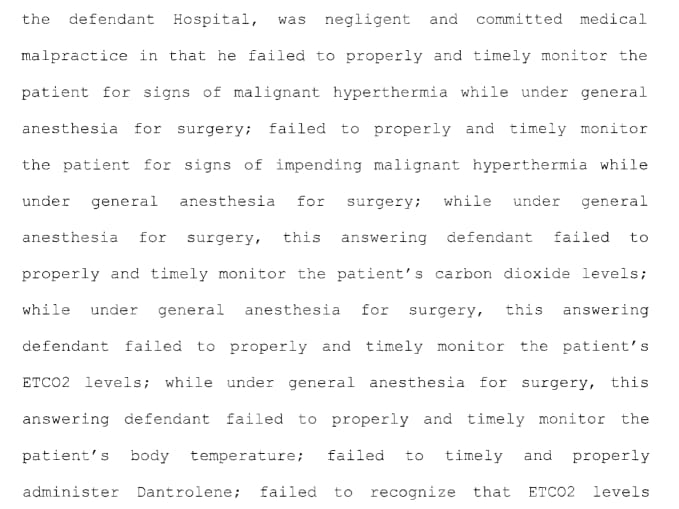
The plaintiff’s attorney hired an anesthesiology expert who provided the following opinion




Outcome
The defense had submitted their own expert opinion, and argued for dismissal in a motion for summary judgment.
Here is what the judge had to say:
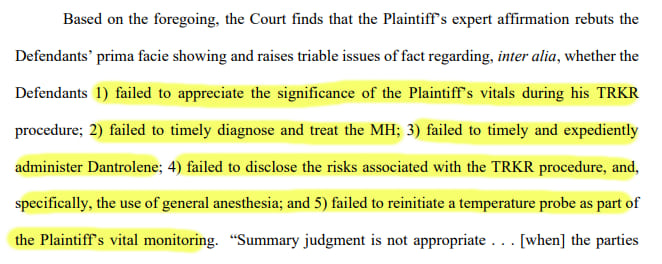
The judge thinks these are all triable issues and therefore must be decided on by a jury.
This comment from the judge was made regarding informed consent.
The case is currently ongoing.
I will update you as it progresses.
Sign up for the email list to be notified when updates occur.
MedMalReviewer/Anesthesiologist Analysis:
I recall thinking there would be some degree of grace given in medical malpractice when a diagnosis is exceedingly rare or difficult. Over the years I have found this is unfortunately not the case, and those in law rarely appreciate how remarkable and unique some of what we encounter is. This is the diagnosis of this anesthesiologists career. He will always remember the patient with MH (and especially now that he’s been sued!).
I have 2 other MH cases at least one of which will be published in the future. In all 3 of these cases dantrolene was given and MH treated. In all 3 the allegations are the same against the anesthesiologist, and the focus of the expert opinion is the same… there was a delay in giving dantrolene. While all cases are different and conclusions can’t be universally applied, this seems to be a primary theme in MH lawsuits. If there are suspicions get to the diagnosis quickly with another opinion in the room, a call to MHAUS, and don’t delay treatment. If there is litigation they will look at when dantrolene was started, and when a reasonable diagnosis could have been made. It won’t be hard to find an expert to opine that reasonable diagnosis immediately follows increasing CO2.
The allegations of a lack of informed consent do not seem appropriate. If patients were consented for every individual possible complication of anesthesia and surgery, consent forms would take hundreds of pages of paper. I certainly have never seen neuroleptic malignant syndrome on a consent. Further, how could the judge write the plaintiff was not aware of another anesthetic option when there was a failed spinal prior to GA conversion? This is at odds with the facts of the case. What other anesthesia option was he referring to? A TIVA discussion? It doesn’t make much sense. I’m trying to get in the judges head and all I can imagine is he knew he would send the case to trial and decided the jury can sort the issue of informed consent out too.
It’s unfortunate MH presented itself during emergence. The temperature probe was taken out of course for wakeup. ETCO2 can jump during emergence. All this made the diagnosis more challenging. I do find it interesting that MH appeared triggered when the tourniquet was released. As if this stress response specifically triggered MH in a susceptible individual, or maybe it’s a coincidence.
Reply